People frequently say that the eyes are the windows to the soul, but in terms of health and addiction, they are also windows to the body’s internal condition. One of the most reliable physical signs that someone is under the influence of drugs is that their pupils change size. A lot of individuals know about the “saucer-eyed” appearance of dilated pupils that come with stimulants, but pinpoint pupils are a very important warning sign for a different kind of harmful medication.
If you are concerned about a loved one, understanding what drugs cause pinpoint pupils can be the first step toward identifying a substance use disorder and seeking help. This guide will explore the biology behind these changes, identify the specific substances responsible, and contrast them with other drug-induced eye conditions.
Why Do Drugs Cause Pinpoint Pupils?
To comprehend the significance of pinpoint pupils, it is essential to examine the autonomic nervous system. The sphincter muscle (which makes the pupil smaller) and the dilator muscle (which makes it bigger) work against each other to govern the size of the pupil.
In normal circumstances, pupils become smaller when there is a lot of light and bigger when there is less light. But putting certain drugs into the body may make these natural responses not work. The most common cause of pinpoint pupils is activation of the parasympathetic nerve system, which controls the body’s “rest and digest” processes.
What does it indicate in medicine when pupils are pinpoint? Clinically called miosis, it means that the pupil becomes too small, sometimes to the size of a pinhead (less than 2 millimeters). When drugs stimulate certain receptors in the brain, including the opioid receptors, they send a signal via the parasympathetic nerves to the iris sphincter muscle, which closes it. This gives the “pinned” effect that doesn’t shift with changes in illumination.
What Drugs Cause Pinpoint Pupils?
When asking what drugs cause pinpoint pupils, the answer almost exclusively points toward a specific and dangerous class of substances: opioids. However, there are a few prescription medications and toxins that can also produce this effect.
Opioids
Opioids are the primary answer to what drugs cause small pupils. These powerful depressants interact with the opioid receptors in the central nervous system to block pain and induce euphoria. A side effect of this interaction is severe miosis. If you notice someone with pupils that look like tiny black dots, they may be using one of the following:
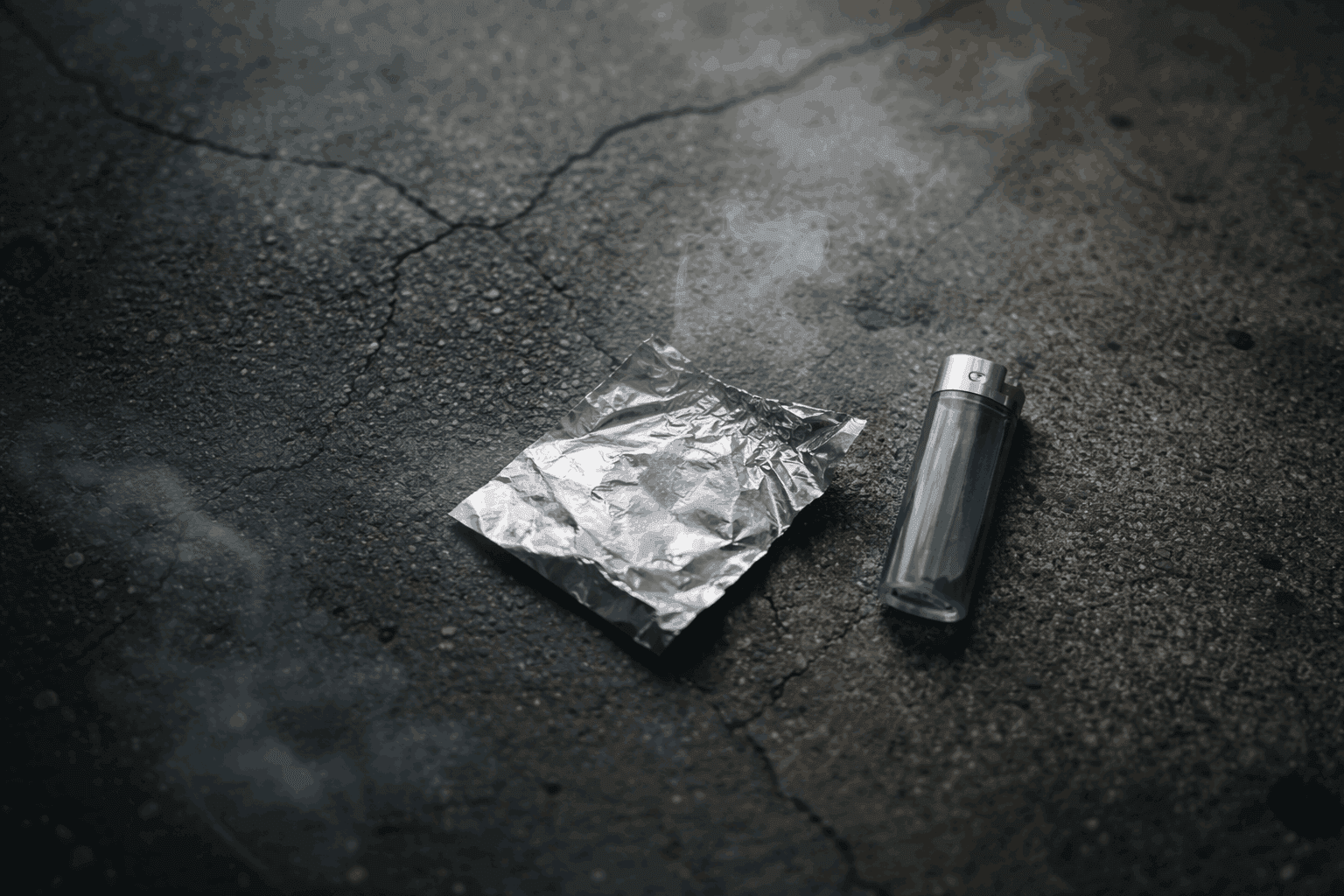
- Heroin: Perhaps the most infamous cause, heroin induces rapid and severe pupil constriction.
- Fentanyl: A synthetic opioid 50 to 100 times more potent than morphine; even tiny amounts cause pinned eyes.
- Prescription Painkillers: Medications like Oxycodone (OxyContin), Hydrocodone (Vicodin), Morphine, and Codeine.
- Methadone and Suboxone: Even medications used to treat opioid addiction can cause miosis.
Because the constriction is caused by the drug’s direct effect on the brain, the pupils will remain small even in a dimly lit room, which is a major red flag distinguishing drug use from normal physiological responses.
Hypertension Medications (Clonidine)
Opioids are the most prevalent cause of pinpoint pupils, however they are not the only ones. Clonidine is a medicine that is mostly used to treat high blood pressure (hypertension) and occasionally ADHD or drug withdrawal. It may also produce miosis.
Clonidine acts by activating alpha-2 adrenergic receptors in the brain, which slows down sympathetic outflow. The parasympathetic system takes over when the sympathetic system is less active, which makes the pupils smaller. Clonidine usage is less prevalent than opioid misuse, however it occurs, sometimes in conjunction with other medications to enhance their effects.
Other Depressants and Toxins
There is often confusion regarding pupils on different drugs, specifically sedatives. For example, while benzodiazepines are depressants, they do not typically cause pinpoint pupils on their own. However, there are other chemical agents:
- Barbiturates: In rare cases of high-dose toxicity, barbiturates can cause pupil constriction, though they are less consistent than opioids.
- Organophosphates: Found in insecticides and nerve agents, these toxins cause severe miosis as part of a “cholinergic crisis,” often accompanied by drooling and tearing.
Identifying Substance Abuse: Pinpoint Pupils vs Normal
Recognizing the physical signs of drug use requires a keen eye. Comparing pinpoint pupils vs normal eyes can help you determine if immediate medical intervention or addiction treatment is necessary.
What do Pinpoint Pupils (Myosis) look like?
Pinpoint pupils meaning is literal: the black center of the eye shrinks to a tiny dot. In a person who is sober and healthy, pupils will naturally fluctuate in size. In someone under the influence of opioids, the pupils will be:
- Fixed: They do not dilate even when the light is low.
- Unresponsive: They may not react quickly to changes in light intensity.
- Glassy: Often accompanied by a glazed or drooping appearance of the eyelids (nodding off).
This look is the direct opposite of dilated pupils. If you walk into a dark room and the person’s pupils do not expand to let in more light, but remain constricted, this is a strong indicator of opioid use.
What do Dilated Pupils (Mydriasis) look like?
To fully understand eyes on different drugs, it is helpful to know what the reverse looks like. Many illicit substances cause mydriasis, where the pupil consumes almost the entire iris.
- Cocaine Eyes: Stimulants like cocaine flood the brain with dopamine and norepinephrine, triggering the “fight or flight” response and causing massive pupil dilation. Cocaine eyes are often wide, alert, and accompanied by rapid blinking.
- Meth Pupils: Similar to cocaine, methamphetamine causes significant dilation. Meth pupils can remain dilated for long periods, often up to 24 hours, giving the user a startled or intense stare.
- Molly Eyes (MDMA/Ecstasy): MDMA is notorious for causing saucer-like pupils. Molly eyes are a hallmark of the drug, often so dilated that the colored iris is barely visible.
- Pupils on Xanax: There is frequent confusion here. Unlike opioids, pupils on Xanax (benzodiazepines) are typically normal or slightly dilated. They are rarely pinpoint unless combined with opioids (a dangerous combination). Users may have “glassy” eyes or heavy lids, but they do not typically exhibit the severe miosis seen in heroin use.
Understanding what drugs cause small pupils versus what drugs cause large ones allows you to narrow down what substance a person might be using.
Risks and Dangers of Pinpoint Pupils
Pinpoint pupils are not just a cosmetic change; they are a sign that the body’s central nervous system is significantly depressed. The biggest danger associated with pinpoint pupils overdose is respiratory failure.
When a person takes a high dose of opioids, the same mechanism that constricts the pupils also tells the brainstem to slow down breathing. If you see someone with pinpoint pupils causes for concern immediately, especially if they are also exhibiting:
- Pale, blue, or clammy skin.
- Slow, shallow, or gurgling breathing (the “death rattle”).
- Unconsciousness or inability to wake up.
- Limp body.
Pinpoint pupils overdose is a medical emergency. If you suspect an opioid overdose, administering Narcan (naloxone) can reverse the effects, including the pinpoint pupils, almost immediately.
Treatment Options for Substance Use Disorder
Identifying what drugs cause pinpoint pupils is often the moment a family member realizes the severity of the situation. Whether the cause is prescription painkillers, heroin, or fentanyl, the presence of fixed, constricted pupils is a sign of physical dependence that requires professional treatment.
We at The House of Life know that addiction is a complex condition that affects the brain and body in many ways. Our evidence-based treatment programs are meant to help people safely get rid of drugs and alcohol and learn the skills they need to stay sober for a long time.
Don’t wait if you see the indications of cocaine eyes, meth pupils, or the pinpoint pupils of opioid addiction in someone you care about. Intervening early can save lives.
Getting over an opioid addiction is hard because of the terrible withdrawal symptoms, but it is doable with the correct therapy.
- Medical Detoxification: The first step for those exhibiting chronic pinpoint pupils is often detox. Medical professionals monitor vital signs and may use tapering schedules to safely manage agonizing withdrawal symptoms like nausea, cramping, and anxiety.
- Medication-Assisted Treatment (MAT): Considered the “gold standard” for opioid disorders, MAT combines therapy with medications. Suboxone and Methadone reduce cravings and normalize brain function without the high, while Vivitrol blocks opioid effects entirely.
- Inpatient Residential Treatment: Severe addiction often requires 24/7 care to remove individuals from triggers. Facilities like The House of Life provide structured environments and holistic care (nutrition, mindfulness) alongside traditional medical support.
- Behavioral Therapies: Detoxification is focused on the body, while therapy works on the mind. Cognitive Behavioral Therapy (CBT) helps change negative thinking patterns. Group and Family Therapy, on the other hand, develop community support and fix relationships.
- Outpatient & Aftercare: Recovery is a lifelong journey. Partial Hospitalization (PHP) and Intensive Outpatient Programs (IOP) offer flexibility, while Sober Living Homes and 12-step programs like Narcotics Anonymous provide long-term accountability.
Resources:
Dhingra D, Kaur S, Ram J. Illicit drugs: Effects on eye. Indian J Med Res. 2019 Sep;150(3):228-238. doi: 10.4103/ijmr.IJMR_1210_17. PMID: 31719293; PMCID: PMC6886135. https://pmc.ncbi.nlm.nih.gov/articles/PMC6886135/
Roth, E. (2018, May 2). What to know about traumatic brain injury. Medical News Today. https://www.medicalnewstoday.com/articles/321209