Dual Diagnosis Treatment Center
Among a wide range of treatment options, individuals with addiction and substance use disorder may find it overwhelming to find the right recovery choice. At The House of Life, you’ll get an array of treatment programs, addressed to each client’s unique needs.
Scroll
Addiction and mental health challenges aren’t merely concurrent; they forge a self-sustaining feedback loop, each condition fueling the other’s persistence. Disentangling this internal dynamic necessitates a bespoke approach. Our center for Co–Occurring Disorders is precisely engineered for this purpose: championing the indivisible integration of therapeutic interventions. Our bespoke program acts as a meticulously synchronized intervention, strategically engineered to disrupt the foundational mechanisms driving both conditions. We provide the complete clinical ecosystem essential for transformative recovery.
What Is a Dual Diagnosis?
More than just two diagnoses on paper, a dual diagnosis represents a profound confluence of challenges: a substance use disorder and a distinct mental health condition, where each exerts a significant, compounding influence on the other. This dynamic is rarely a straightforward cause-and-effect; rather, it unfolds as a relentless, reciprocal loop. Envision someone attempting to silence intense panic attacks with a benzodiazepine, inadvertently constructing a physical reliance that, in turn, paradoxically heightens their baseline apprehension.
Conversely, the damaging neurological footprint of prolonged substance use can serve as a potent accelerant, transforming a dormant psychological predisposition into an undeniable, full-blown disorder. Piecemeal treatment, which attempts to separate these inextricably linked conditions, is fundamentally insufficient, as the neglected aspect invariably undermines any therapeutic gains. True, enduring stability necessitates a singular, integrated treatment strategy expertly devised to master this intricate landscape.
Common Co Occurring Disorders
When psychological distress and substance dependency intersect, they create a complex, self-reinforcing dynamic. Though every individual’s journey is distinct, specific combinations of these conditions tend to appear together. Recognizing the specific blueprint of this interaction is fundamental to developing a truly targeted and successful therapeutic strategy.
Depression and Alcohol Dependence:
For those battling depression, alcohol can present a deceptive promise of relief. Initially, it may seem to numb the persistent feelings of emptiness or sadness. However, because alcohol is a powerful central nervous system depressant, its use actively disrupts crucial neurochemistry, ultimately deepening the shadows of the original depressive episode and creating a powerful cycle of dependency.
Anxiety Disorders and Sedative Misuse:
The relentless distress of anxiety can lead to sedative use (e.g., benzodiazepines) for rapid relief. This often induces a physiological dependence, where the body requires the drug to function. Ironically, this dependency heightens the brain’s innate anxiety, worsening the original condition.
Post-Traumatic Stress Disorder (PTSD) and Substance Use:
PTSD creates a perpetual state of high alert. Substances are often used as a flawed coping mechanism to mute intrusive memories, lower hypervigilance, or numb emotional pain. This offers only a temporary chemical reprieve, not a resolution, often deepening the trauma cycle.
Bipolar Disorder and Substance Use:
The volatile swing between manic and depressive states drives self-medication. Stimulants may be used to counter depression, while sedatives aim to manage mania. These attempts at chemical regulation severely disrupt neurological balance, intensifying mood instability.
ADHD and Stimulant Misuse:
While central to treatment, prescription stimulants carry misuse risk. Some escalate doses for heightened focus or euphoria. Others may use different substances to self-manage symptoms like impulsivity and restlessness, often complicating their clinical picture.
Recognizing the Need for Help:
Achieving diagnostic clarity is often complicated by the fact that the two conditions are locked in a feedback loop, where the manifestations of one can either conceal or intensify the other.
Signs of Mental Health Disorder
- Persistent feelings of sadness, worry, or emptiness.
- Extreme mood swings, from high energy to severe low periods.
- Withdrawing from friends, family, and social activities.
- Major changes in sleep patterns or appetite.
- Difficulty thinking clearly, focusing, or making decisions.
- Hearing or seeing things that others do not.
- Thoughts of harming yourself or others.
Signs of Substance Use Disorder
- Developing a need for larger amounts to achieve the same impact, as your body adapts over time.
- Experiencing physical or emotional distress, such as nausea, anxiety, or restlessness, when you try to quit or reduce use.
- Repeatedly trying and failing to limit or stop consumption, even when you genuinely want to.
- Devoting significant time and energy to obtaining, consuming, or recovering from the effects of the substance.
- Falling behind on obligations, whether at work, in school, or within your personal life, because of substance use.
- Persisting with use even when it causes harm to your well-being, strains relationships, or creates financial difficulties.
- Losing interest in hobbies, passions, or social activities that once brought you joy, replacing them with substance use instead.

How Is Dual Diagnosis Diagnosed?
To ensure an accurate diagnosis, our process synthesizes information from multiple sources, creating a holistic view of your well-being.
- Expansive Biopsychosocial Interview:
We begin with a detailed conversation that delves into your unique life story, encompassing personal background, current life circumstances, historical and current relationship with substances, family history and dynamics, as well as past traumatic experiences. This narrative is vital for contextualizing your present challenges.
- Objective Symptom Quantification:
Our clinicians utilize established, norm-referenced psychological instruments to impartially detect and gauge the intensity of clinical symptoms. This empirical approach adds a critical data-driven layer to our assessment.
- Physiological Health Review:
A cornerstone of our process involves a physical health evaluation, which includes laboratory analysis. This step is crucial for discerning whether symptoms might stem from underlying medical issues – such as hormonal dysregulation or neurological factors-that can produce mental health manifestations.
- Disentangling Co-occurring Conditions:
A central analytical focus is differentiating between transient symptoms attributable to substance use (which typically abate with detoxification) and those stemming from a separate, foundational psychiatric condition. Securing this diagnostic clarity is the crucial first step in formulating a targeted and sustainable path to recovery, designed specifically for your situation.
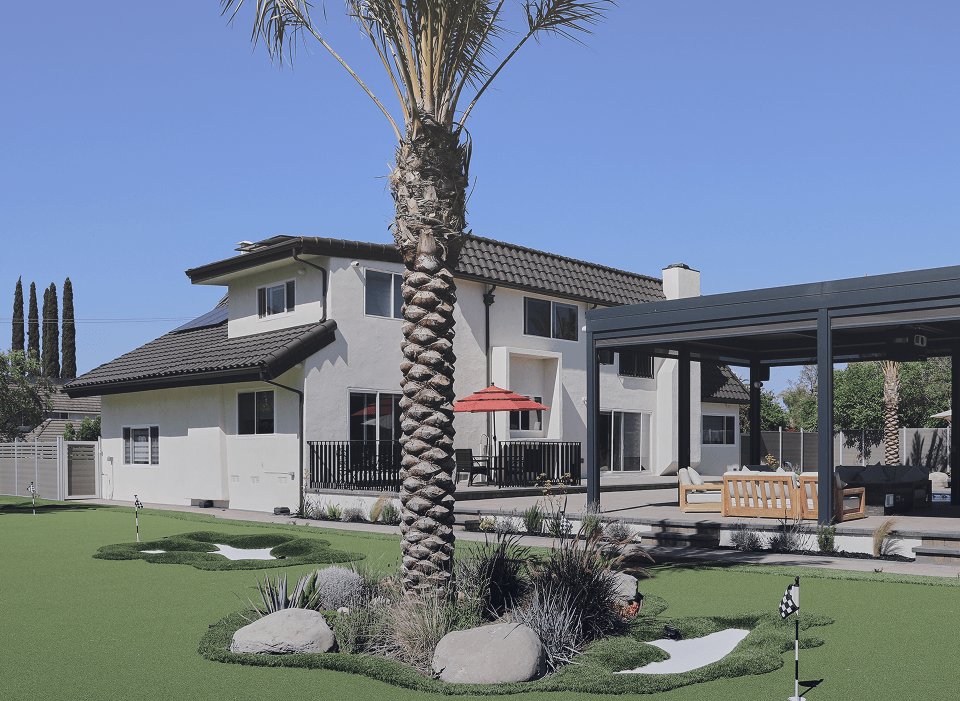
Our Approach to Dual Diagnosis Treatment
We operate from the deep understanding that addressing interconnected health issues demands more than isolated interventions. Our rehab is founded on the principle of cohesive, person-centered care, embracing you in your totality, rather than segmenting your struggles. Our facility itself embodies this philosophy, intentionally structured to ensure your full spectrum of support—from mental health experts to holistic practitioners
Integrated Care for Mental Health and Addiction
We challenge the outdated notion of separate care for addiction and mental health. At The House of Life, they are unified priorities, always addressed in concert. Your therapist and prescribing clinician function as a cohesive unit. Our medication management strategy isn’t solely about symptom reduction; it’s about achieving neurological harmony, paving the way for a mind calm enough to delve into the transformative, root-cause resolution work of psychotherapy. Experience truly integrated healing.
Evidence-Based Therapies
Our clinical methodology is driven by interventions with demonstrated efficacy for dual diagnoses. We move beyond generic application, expertly tailoring these modalities to disrupt the specific feedback loops between your conditions.
- Cognitive Behavioral Therapy (CBT): Our clinicians specialize in helping you deconstruct the self-defeating thought patterns that automatically trigger both emotional distress and addictive behaviors. You will learn to challenge and reframe these cognitions, building a more resilient and rational mindset.
- Dialectical Behavior Therapy (DBT): We provide a robust skill-set for managing emotional volatility. This includes practical training in distress tolerance to survive crises without relapse, mindfulness for present-moment awareness, and interpersonal effectiveness for building healthier relationships.
- Motivational Interviewing (MI): Our therapists act as guides to help you navigate and resolve internal ambivalence about change. This collaborative process strengthens your own personal drive and commitment to recovery, making your goals self-directed rather than imposed.
- Trauma-Informed Therapies: Our entire clinical approach is built on an understanding of trauma’s neurobiological impact. We employ modalities like EMDR and somatic experiencing to safely process and integrate traumatic memories, reducing their power to trigger symptoms and substance use.
Multidisciplinary Team Support
You are supported by a dedicated team that communicates daily. This team includes:
- Psychiatrists & Addictionologists
- Licensed Therapists and Counselors
- Registered Nurses
- Case Managers
- Wellness Specialists
Holistic and Wellness Programs
True healing extends beyond traditional therapy. We incorporate practices that heal the mind and body together:
- Mindfulness and Meditation
- Yoga and Fitness
- Nutritional Counseling
- Art and Recreation Therapy
Dual Diagnosis Treatment Programs We Offer
We provide a full continuum of care, allowing you to move through different levels of support as you grow stronger.
Residential Inpatient Care
For those requiring a foundational level of stability, our residential inpatient program provides a secure and immersive healing environment.
This comprehensive care model removes you from daily triggers and provides unwavering 24/7 medical and therapeutic support. Within this structured setting, you can fully focus on initial recovery goals, achieve physiological stabilization through monitored detoxification, and begin your therapeutic work in a safe space. It represents the most intensive level of care we offer, creating the essential bedrock for all subsequent healing.
Partial Hospitalization Program (PHP)
Serving as a vital transitional step, our Partial Hospitalization Program (PHP) delivers the rigorous clinical engagement of inpatient care with the autonomy of returning home each night.
Patients participate in structured, multidisciplinary therapy for several hours during the day, five to seven days a week, before applying their new skills in their home environment. This program is ideally suited for individuals transitioning from residential treatment or for those who require significant support to avoid hospitalization altogether, offering a critical balance of intensive care and personal independence.
Intensive Outpatient Program (IOP)
For clients who have established a foundation in recovery but require ongoing structure to navigate the complexities of daily life, our Intensive Outpatient Program provides vital support. The IOP is specifically structured to integrate with your ongoing professional, educational, and family commitments. Participants attend focused therapeutic sessions multiple times per week to equip them with the resilience needed to manage real-world triggers and stressors. The program’s core focus is on fostering the advanced emotional regulation skills essential for long-term success in managing co-occurring conditions, all within a collaborative and encouraging peer setting.
Aftercare and Relapse Prevention
Our commitment to your well-being extends far beyond the completion of a primary treatment program. To ensure a successful and lasting transition into daily life, we develop personalized continuing care blueprints. These strategic roadmaps include regular one-on-one sessions for accountability, connections to specialized peer support networks, and engagement with our active alumni community.
Our case managers act as dedicated recovery allies, assisting with practical challenges like vocational planning, securing stable sober housing, and connecting you to vital community-based resources. This creates a durable scaffolding for a new life, ensuring you have a robust safety net for your ongoing journey.
What to Expect During Treatment
Knowing what to expect can ease anxiety about starting treatment. Your journey will typically follow these phases:
Phase 1: Intake & Stabilization.
You’ll undergo a thorough assessment, and our medical team will ensure you are physically and psychologically stable, often beginning with a detox protocol if needed.
Phase 2: Active Treatment & Skill Building.
You will engage deeply in individual, group, and family therapies. You’ll learn practical skills to manage cravings, regulate emotions, and challenge destructive thoughts.
Phase 3: Transition & Aftercare Planning.
As you prepare to leave, we focus on solidifying your relapse prevention plan, connecting you with outpatient resources, and ensuring a confident transition back to your daily life.
Is Dual Diagnosis Treatment Effective?
Integrated Dual Diagnosis Treatment is the only modality proven to achieve sustainable outcomes for co-occurring disorders. Its critical importance is highlighted by a stark reality: most conventional programs, which treat addiction and mental health in isolation, are structurally unequipped to manage their complex interaction, leading to a high rate of treatment failure and relapse.
Why Our Integrated Model Delivers Superior Results:
Synchronized Intervention: This methodology shatters the cycle of reciprocal influence by concurrently addressing both disorders within a unified therapeutic blueprint, facilitated by a singular, cohesive clinical team.
Profound Etiological Healing: The approach transcends mere symptom management, instead delving into the foundational trauma, emotional distress, and neurological patterns that inherently fuel both conditions.
Enduring Stability Framework: By empowering individuals with robust strategies for navigating mental health triggers, the model directly diminishes the vulnerability to substance relapse, thereby forging a significantly more resilient recovery trajectory.
Evolving Therapeutic Journeys: Treatment here is never a static, off-the-shelf program. It unfolds as a responsive, adaptable plan that matures alongside the individual, meticulously targeting unique personal histories and aspirations.
Dual Diagnosis Treatment Center: FAQ
What Is the Treatment for a Dual Diagnosis?
What Is the New Term for Dual Diagnosis?
What Is the Most Effective Treatment for Dual Diagnosis?
What Is the Downside to Residential Treatment Centers?
Sources:
- Drake R, Mercer-McFadden C, Mueser K, et al. Review of integrated mental health and substance abuse treatment for patients with dual diagnosis. Integrated Mental Health and Substance Abuse. 1998;24(4):589–605. doi: 10.1093/oxfordjournals.schbul.a033351. [DOI] [PubMed] [Google Scholar][Ref list]
- National Alliance on Mental Illness. (2017, October). Dual diagnosis [Fact sheet]. Retrieved September 9, 2025, from https://www.nami.org/NAMI/media/NAMI-Media/Images/FactSheets/Dual-Diagnosis-FS.pdf
- National Alliance on Mental Illness. (2017, October 4). Understanding dual diagnosis. Retrieved September 9, 2025, from https://www.nami.org/advocate/understanding-dual-diagnosis/
- Substance Abuse and Mental Health Services Administration. (2002). Chapter 1: Uniform criteria for patient placement [Archived webpage]. Internet Archive. Retrieved September 9, 2025, from https://web.archive.org/web/20120501034913/http://www.samhsa.gov/reports/congress2002/chap1ucod.htm